STAGE 1: NO SIGNS OF DECLINE
The only way to detect dementia this early is if tests are run by a doctor that reveal the beginnings of dementia.

If your loved one has been diagnosed with dementia, you’re probably asking a lot of questions.
What exactly is dementia?
Is it the same as Alzheimer’s?
What symptoms come with a dementia diagnosis?
And, what happens during dementia?
What should I know about memory care?
When should I consider a memory care facility?
With this often misunderstood diagnosis, it’s understandable you would be asking these questions.
Dementia itself is not a specific disease but refers to a general loss of memory, language, or problem-solving skills and other difficulties associated with the part of the brain that controls these functions.
The effects of dementia reveal themselves more slowly over time. There are generally seven stages that move from mild to severe.
Dementia is not the same as Alzheimer’s disease. Dementia is an umbrella term that includes Alzheimer’s disease as well as vascular dementia, frontotemporal dementia, and Lewy body dementia.
Alzheimer’s makes up 60-80% of dementia cases, so the two are often confused.
Symptoms of dementia include short-term memory loss, confusion, misplacing items, forgetting appointments, struggles with communicating, among others. Symptoms vary depending on the person, medical history, and current health status.
Dementia is caused by damage to brain cells. Typically this damage is irreversible and deteriorates over time until brain cells can no longer communicate with one another, causing severe loss of basic functions such as walking and eating. Sometimes what is thought to be a dementia symptom like memory loss, is instead caused by depression, a medication side effect, a thyroid problem, or a vitamin deficiency, in which case the damage is usually reversible with treatment.
Dementia can be broken down into two categories: cortical dementia and subcortical dementia.
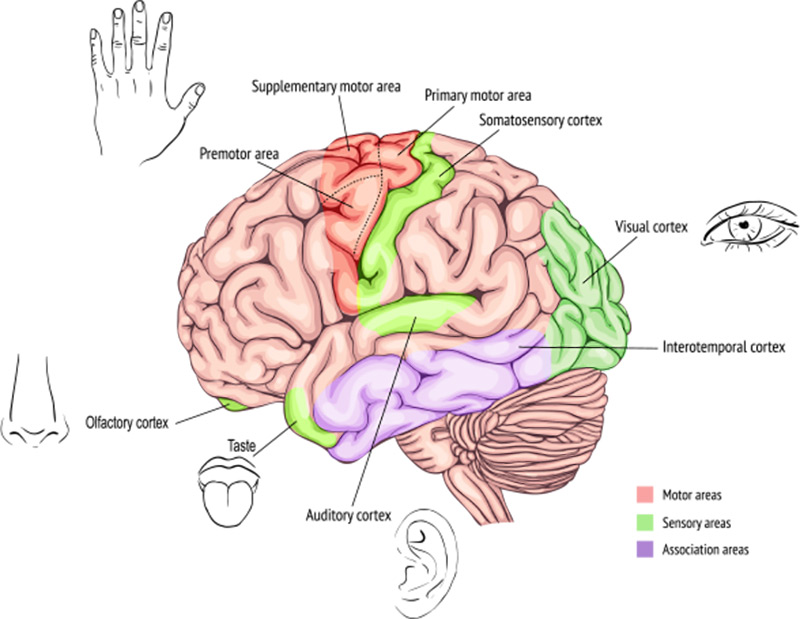
Cortical dementia affects the outer layer of the brain, known as the cerebral cortex. This causes problems with memory and language because the cerebral cortex is largely responsible for these functions. Alzheimer’s disease is a type of cortical dementia.

Subcortical dementia affects parts of the brain beneath the cortex.
People with this type of dementia may not experience the same language and memory problems as those with cortical dementia, but they will have problems with starting activities, or they may suffer from slower than usual thinking.
Dementia works in stages.
Someone with dementia will not suddenly lose her short-term memory or show severe language impairment. The effects of dementia reveal themselves more slowly over time. There are generally seven stages that move from mild to severe.
The only way to detect dementia this early is if tests are run by a doctor that reveal the beginnings of dementia.
Your loved one is still able to live independently but you will notice signs of decline in their memory, speech, or language.
You will notice more issues with your loved one’s memory, planning skills, and reasoning. They may start to repeat themselves at this stage.
Remembering recent events (short-term memory) will become more difficult at this stage.
At this stage, a person will have more obvious challenges with memory, forgetting things like their grandchild’s name, what day it is, or what time it is. This is when everyday assistance may be needed.
Memory loss becomes more severe at this stage. Many people may forget their spouse’s name, and they will probably need help going to the bathroom, eating, and walking.
At this stage, your loved one will no longer be able to speak clearly or walk on his own. He will need assistance with all activities of daily living.
Dementia can be incredibly difficult for the person diagnosed as well as the caretaker as you brace yourself for each stage of decline. That is the nature of the degenerative disease.
But just because dementia—and the diseases that fall under its umbrella—are degenerative, does not mean there isn’t hope for those who have them.
As mentioned earlier, some cases of dementia are reversible. Tumors, thyroid imbalance, hormonal imbalance—all of these can cause dementia but are treatable illnesses. When the tumor is removed or balance is restored to the body, the dementia symptoms will go away.
In addition, the FDA recently approved a drug for Alzheimer’s disease called Aduhelm. It’s the first FDA-approved drug for Alzheimer’s in several decades. Aduhelm is a drug infusion that may lessen the build-up of plaque in the brain that is associated with memory loss. Unfortunately, this drug has not been shown to have any significant effect on cognition.
Usually, doctors will try and treat or reduce the symptoms of whatever is causing their dementia. Proper nutrition, exercise, and a strong sense of community are all helpful for people with various forms of dementia. While they are not a cure, they are something any caretaker, friend, or family member can offer a loved one who has been diagnosed with memory loss.
To learn more about dementia, Alzheimer’s, and how you can help your loved one, visit our resources page here.

Call us for more information
Barton House Sugarland
Have more questions?
Want to see our facility?
Want to recieve updates?
`

As the coronavirus (COVID-19) pandemic continues to evolve, our communities are focused on keeping our Residents and staff safe while also maintaining Resident engagement and daily fulfillment. We are taking a cautious approach, balancing the highest level of safety within the least restrictive environment.
We will continue to follow and augment State and C.D.C. safety recommendations:
Screening: We screen every employee every day. We require our staff to complete a questionnaire (inquiring about possible symptoms, recent travel and exposure), have their temperature and oxygen level checked before entering the building. Staff are also required to clean their cell phones, keys and wash their hands while being observed. We monitor our Residents’ health closely with temperature and oxygen level checks at least twice a day. We help our Residents wash their hands throughout the day and encourage them to wear a mask or face covering.
Cleaning: We have enhanced our cleaning products with regard for their effectiveness in killing COVID-19 particles and proper sanitization and disinfection, using the EPA’s specific list of disinfectants for use against the coronavirus. We are using this list and training staff on how long cleaning solutions must be kept on a surface before wiping it off to ensure its effectiveness. We prioritize cleaning high-touch areas and horizontal surfaces, cleaning them several times a day.
Physical Distancing: We encourage 6 foot distancing between Residents and with staff unless they are providing direct care to a Resident.
Testing: We test all Residents and staff for COVID-19 every three weeks, and more as needed. Our nurses utilize a PCR test, which we send to a private lab to expedite results.
Physical Changes: We have installed ultraviolet lights in our air conditioners that supply air to the common areas of the houses. This method is believed to be helpful in killing bacteria that is cycled through the systems and pushed back into the house. We’ve also enhanced our HVAC filters to near HEPA levels, trying to add additional layers of protection to keep COVID-19 out of the building. Most importantly, air purifiers have been added to common areas and each resident room.
PPE: Staff members wear masks at all times and we encourage Residents to wear masks when outside their rooms. We also encourage physical distancing between our Residents. Staff wears additional protective equipment when deemed necessary while caring for our Residents. Staff are continually trained on when and how to use personal protective equipment (PPE).
The uncertainty surrounding COVID-19 affects us all. At our communities, we are not letting it stop us from safely offering a life well-lived. Above all, we are providing the utmost attention to the safety and well-being of our Residents. Our Program has always revolved around the individualized needs of each Resident and this has not changed during COVID-19. Residents are still able to connect with each other and staff while maintaining a safe physical distance. Weather permitting, we enjoy the patio and large backyard. We continue to keep our Residents engaged through cognitive, physical, recreational experiences. We offer enjoyment and connection throughout the day even during these unprecedented times.
Since early March we have restricted facility access to prevent the spread of COVID-19.
Essential Visitors: Healthcare providers including physicians, home health, private duty services, physical therapy and hospice staff have not been allowed in the communities unless there is an acute, essential need for our Residents. These services continue as needed through FaceTime, tele-med and phone conversations. If physical access is absolutely necessary, the individual will complete our questionnaire and screening for temperature and oxygen stats. No one is allowed in the community if they fail to meet our screening criteria.
Families: We are happy to help schedule window visits, FaceTime, Zoom and phone calls with your loved ones based on what is allowed and prudent. To ensure the proper support from our staff, our visits are scheduled ahead of time.
Tours: We recognize that regardless of the changes with COVID-19, your need for senior living hasn’t changed. For the safety of you, our Residents and staff, we are currently offering virtual tours where you can see our community, as well as meet our staff. Please contact our Community Relations Director to set up a virtual tour.
Move-Ins: We are accepting a limited number of move-ins (unless otherwise instructed by public health department). New Residents must be tested for COVID-19 prior to move-in. Upon admission, we will place a new resident in their room to quarantine as an additional precaution.
We will share community-specific information with residents and families as our quarantine measures continue to evolve with new information of COVID-19.
We are honored to care for your family member and loved one.
“We appreciate all of your efforts. Your team clearly is a leader in the response to COVID. Thank you for keeping our loved ones safe.”
Joseph
“Thank you, thank you, thank you for ALL you have done and are doing to keep the residents and staff in a safe environment! The continuous learning and improvements empower caregivers and families to do better at home and in our communities.”
Tommy
“I appreciate you taking the time to update us and share them with my family living in AL, GA, VA, MD, FL…we are extremely grateful and comforted by your proactive and decisive measures! We’ll continue to keep you in prayer for health, safety and more.”
Rebecca
“In keeping with the parade theme you had, the employees there are super heroes. They are plowing forward in the midst of this horrible virus and taking care of their patients selflessly. I just wanted to acknowledge their bravery and dedication and thank them from the bottom of my heart for the goodness in their hearts and their dedication to their patients and jobs.”
Abigail
“Thank you! You locked down early & your diligence has paid well.
The Bader support group continues meeting once a month by Zoom. We all appreciate you so much. Everyone comments on how grateful we are that our parents are at Barton House!
We appreciate everything: sending us pictures, calls, alerts to bring supplies/clothes as needed, staying in virtual contact with hospice.
Blessings to each of you.”
Marsha
“Thank you for all y’all and all the staff are doing for my mom and the other residents. We truly appreciate your hard work.”
Carol

Receive our weekly newsletter. It’s filled with expert advice to help you learn about the latest in memory care, dementia care, and Alzheimer’s disease. We won’t send you any spam and you can unsubscribe at any time.