Which Is Worse: Dementia or Alzheimer’s?

Which is worse, dementia or Alzheimer’s?
More than six million Americans are living with Alzheimer’s disease, but that doesn’t mean there aren’t misconceptions about what Alzheimer’s disease is and what dementia is. Because of this, you may think of Alzheimer’s and dementia as two separate diseases with different causes and symptoms, leading you to wonder: which is worse—dementia or Alzheimer’s?
But dementia and Alzheimer’s can’t be compared in this way. To understand why, you must understand what dementia is, what Alzheimer’s is and how they’re inextricably linked.
What is dementia?
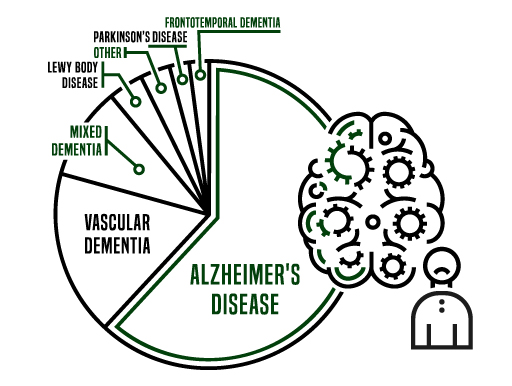
Dementia is not a disease in and of itself but rather a condition that describes a group of symptoms related to neurodegeneration—a deterioration of cells in the brain.
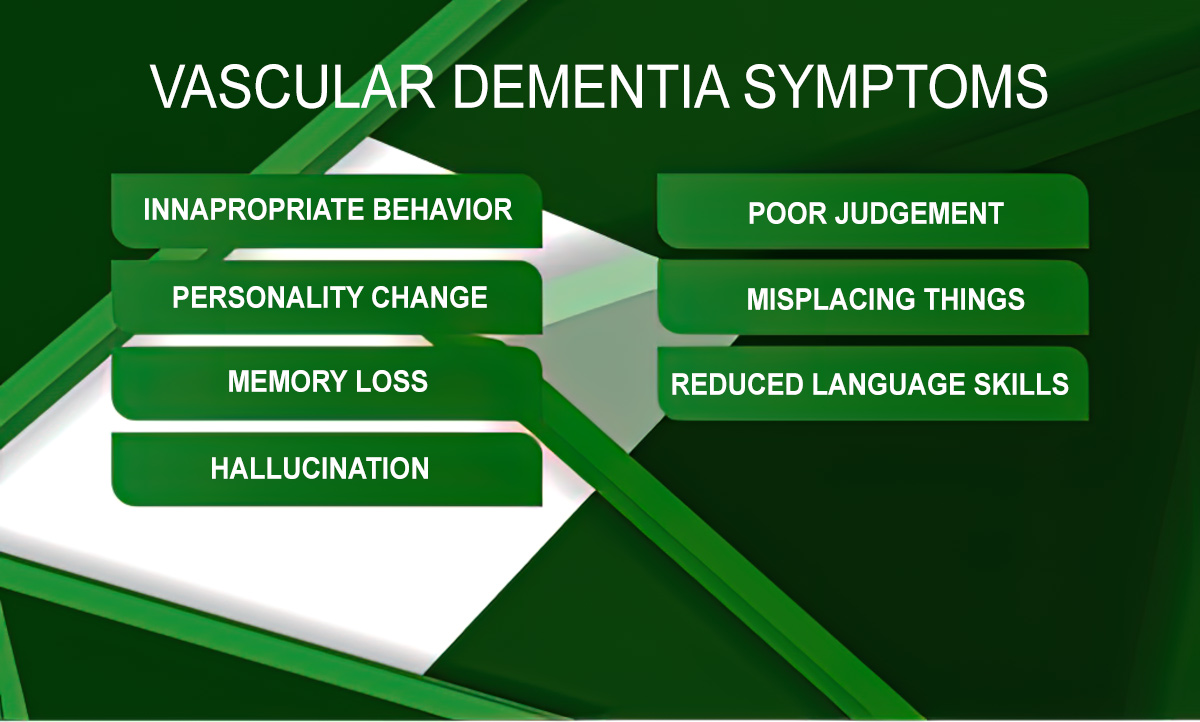
Symptoms of dementia include:
Share this Infographic Image On Your Site
<p><strong>Please include attribution to https://barton-house.com/ with this graphic.</strong><br><br><a href="https://barton-house.com/ways-to-stay-engaged-socially-with-dementia/"><img src="https://barton-house.com/wp-content/uploads/2022/11/barton_house_infographic_Ways_to_Stay-Engage_socially_with_dementia.jpg" alt="Ways to Stay Engaged Socially with Dementia" width="461px"></a></p>Several conditions can cause dementia, including Alzheimer’s disease, which would be considered a type of dementia.
Other types of dementia include:
Let’s take a deeper look at each type of dementia
Huntington’s disease
This type of dementia is hereditary and usually shows up earlier in life, between the ages of 30 and 50. Along with impairing memory and cognitive function, the first symptom of Huntington’s disease is often uncontrollable movement in the upper body.

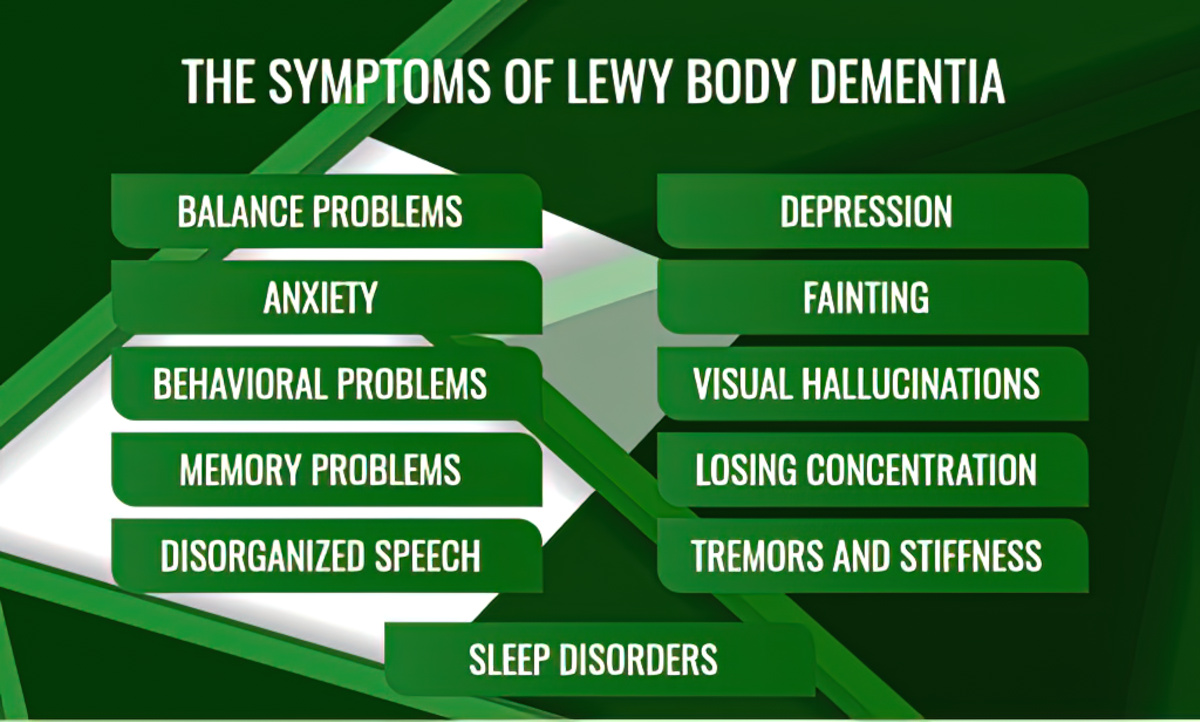
Lewy body dementia
Lewy bodies are abnormal deposits of protein in the brain that cause hallucinations, imbalance in the body and attention issues.
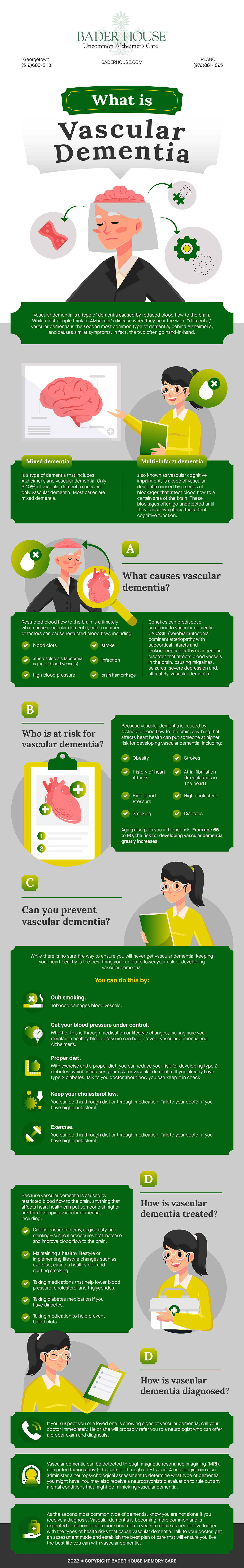
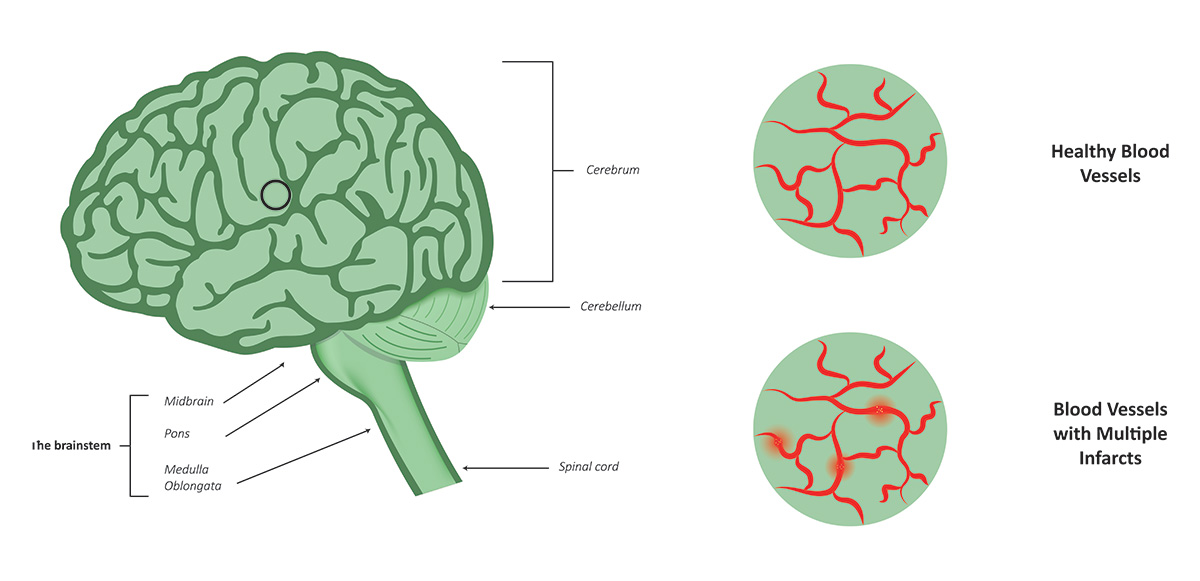
Vascular dementia
Vascular dementia represents 10% of all dementia cases. It’s caused by restricted blood flow in the brain due to blockage in the blood vessels and can lead to stroke or brain bleeds.
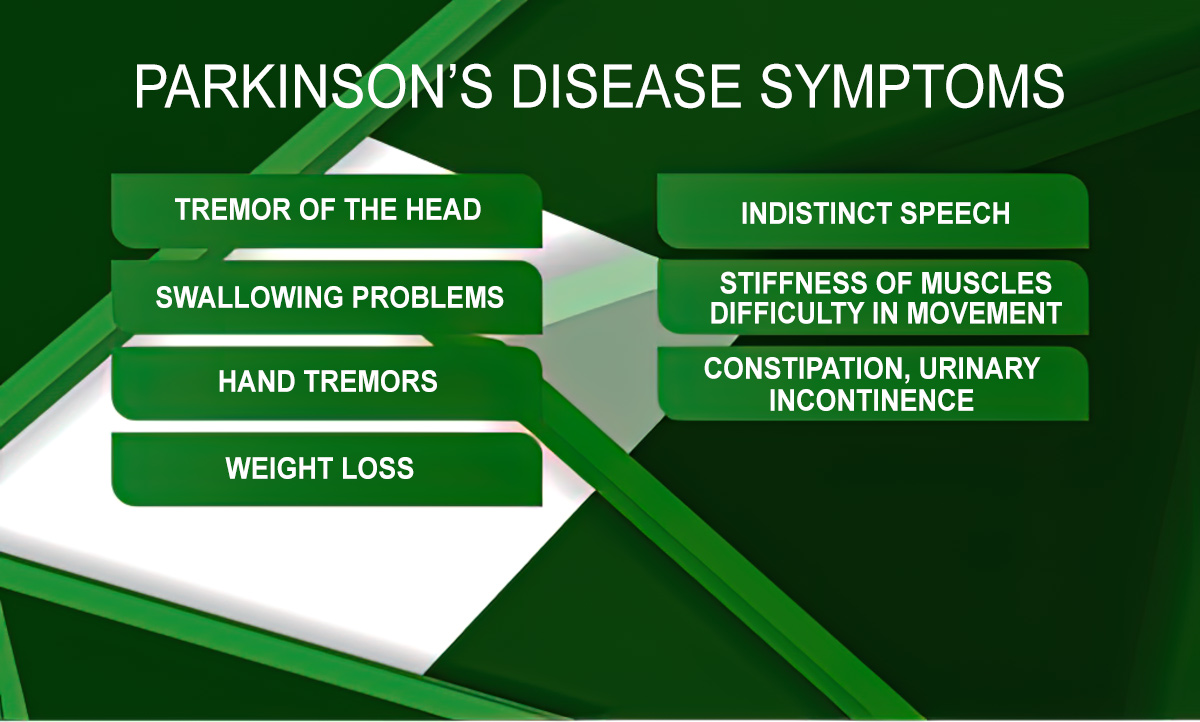
Parkinson’s disease dementia
This type of dementia occurs in those with Parkinson’s disease who also experience a decline in thinking and reasoning skills.
Mixed dementia
When changes in the brain are caused by multiple types of dementia, this is known as mixed dementia. The most common form of mixed dementia is caused by conditions related to Alzheimer’s disease and vascular dementia.
Dementia is not a normal part of aging. Dementia signifies damage has been done to brain cells to the extent that it is interfering with a person’s cognitive function and abilities.
What is Alzheimer’s disease?
Named after physician Alois Alzheimer, who was the first to link memory loss symptoms with changes in the brain, Alzheimer’s disease is the leading disease that causes dementia, causing 60-80% of cases. Because of this, when people talk about dementia, they are often talking about Alzheimer’s disease.
Alzheimer’s is a degenerative brain disease that affects cognitive functions such as memory, learning new information, thinking, reasoning and logic. Symptoms increase and worsen over time.
What are the stages of Alzheimer’s disease
There are five general stages of Alzheimer’s disease. The last three stages are defined by what dementia symptoms are present and to what severity. The length of each stage will vary based on the person, but most will progress through each of these stages in this order.
1. Preclinical Alzheimer’s disease
This stage begins before symptoms of Alzheimer’s, such as memory loss or moodiness, appear. With advanced research, we now know that Alzheimer’s can appear in the brain long before the disease is noticeable to you or others.
Genetic testing, biomarkers, neuroimaging and blood tests can all indicate whether or not someone has Alzheimer’s disease in this stage.
2. Mild cognitive impairment due to Alzheimer’s disease
The Mayo Clinic defines mild cognitive impairment (MCI) as “the stage between the expected cognitive decline of normal aging and the more serious decline of dementia.”[i]
MCI can be caused by Alzheimer’s disease or other conditions such as nutritional deficiencies, autoimmune disease, metabolic imbalance, a brain tumor and more. MCI typically causes issues with thinking, reading, learning, remembering, reasoning and attention span, but it won’t interfere with daily tasks and activities.
Testing can be done to determine if MCI is caused by Alzheimer’s or another condition.
3. Mild dementia due to Alzheimer’s disease
Mild dementia due to Alzheimer’s disease is the stage when Alzheimer’s is most commonly diagnosed because this is typically the stage when symptoms become evident to family members and doctors.
Symptoms of mild dementia due to Alzheimer’s disease include:
Short-term memory loss: difficulty remembering recent events or information
Poor judgment: making poor decisions due to a loss of sound judgment and reasoning skills
Difficulty with problem-solving or completing tasks: an inability to do complex tasks such as balancing a checkbook and an inability to follow through with daily tasks after they are started
Misplacing items: misplacing valuable items more frequently or not being able to remember where they are
Change in personality: withdrawing in social gatherings or feeling angry or irritable more often
Getting lost more frequently: not being able to find once-familiar locations
These symptoms indicate that memory loss and other symptoms have begun to interfere with daily life, making the disease much more prominent and noticeable.
4. Moderate dementia due to Alzheimer’s disease
At this stage of Alzheimer’s, the symptoms that began in the mild dementia stage grow more severe. Memory loss and confusion increase. Basic details about your life such as your birthday may become difficult to remember. Personality and behavior changes are more evident at this stage. Many grow suspicious of their caretakers and loved ones or think they are seeing or hearing things that aren’t there.
At this stage, many may need help with activities of daily life (ADLs), such as going to the bathroom, changing clothes and eating.
5. Severe dementia due to Alzheimer’s disease
Throughout every stage of Alzheimer’s disease neurons in the brain are deteriorating, shrinking the brain. During the final stage of Alzheimer’s, the disease has affected every area of the brain needed for daily functioning, which is why Alzheimer’s is, for now, a fatal disease. This final stage causes those living with Alzheimer’s to not be able to communicate coherently, to need assistance with all ADLs and not be able to physically move or sit up on their own. Eventually, those with severe dementia due to Alzheimer’s will lose their ability to swallow and control their bowels.
Which is worse: Dementia or Alzheimer’s?
Although Alzheimer’s and other types of dementia are ultimately fatal, as research has helped uncover the causes of Alzheimer’s and dementia, treatment has improved as well as a hope for a future cure.
Understanding the connection between dementia and Alzheimer’s is critical in understanding your diagnosis or that of a loved one. One is not “worse” than the other. If you or a loved one is showing signs of dementia, contact your doctor so you can get a proper diagnosis.